Dr. Darren Smith answers all important questions related to arm lift complications in this tell-all.
After massive weight loss or aging, many patients seek brachioplasty for sagging, loose arm skin. But like any surgery, brachioplasty carries risks. What complications should you watch for after your arm lift?
The short answer is there are quite a few like scarring, hematomas, and even blood clots in rare cases. Read on for Dr. Smith’s expert insights on minimizing these issues for optimal results.
What Are Common Brachioplasty Complications?

The most common brachioplasty complications are scarring, fluid accumulation, wound healing issues, skin necrosis, and contour irregularities according to plastic surgeon Dr. Smith’s experience.
- Scarring: Hypertrophic, widened, or unaesthetic scars result in up to 53% of procedures based on studies. Brachioplasty scars are permanent and can become raised, red, or irritated over time. Proper aftercare helps minimize long-term visibility.
- Fluid accumulation: Seromas and hematomas occur in approximately 7% of surgeries according to this study. These fluid buildups under the skin may need drainage or minor surgical intervention. Restricting activity and arm compression early on helps reduce risks.
- Wound issues: Up to 7% of patients experience impaired healing such as wound separation. Risk factors like diabetes and smoking increase the chances of these wound complications. Careful incision care and follow-up helps identify and treat any issues promptly.
- Contour irregularities: Dissatisfaction with aesthetic results and arm symmetry accounts for up to 21% of revision surgeries. Significant weight fluctuations after the initial procedure contribute to asymmetry or shape issues.
While brachioplasty is considered relatively safe, risks of permanent nerve damage, bleeding, and other major complications occur in approximately 3-4% of patients.
Dr. Smith prioritizes careful surgical planning and technique to provide the desired aesthetic results while minimizing risks and complications.
Minimal scarring, maximum results – book your brachioplasty with top NYC surgeon Dr. Smith today.
Can Brachioplasty Issues Be Serious?
Though uncommon, potentially serious brachioplasty risks include major infections, large hematomas, blood clots, severe wound issues, permanent nerve damage, and chronic lymphedema.
- Major infections: Though uncommon, severe infections may require hospitalization for intravenous antibiotics or surgical drainage. Signs like fever or pus signal the need for prompt treatment.
- Hematoma: Bleeding under the skin occurs in around 1-2% of procedures, occasionally necessitating return to the operating room for urgent surgical drainage and control.
- Blood clots: Though rare at 0.4%, venous thromboembolism can happen. Blood clots require immediate medical care to avoid further complications.
- Wound issues: Severe skin necrosis or wound separation leads to disfigurement, impaired function, and poor scarring. These major wound problems may need skin grafts or reconstructive surgery, Dr. Smith advises.
- Nerve injury: While rare, permanent numbness, chronic neuropathic pain, or motor deficits are possible with severe nerve trauma. Most nerve damage resolves over time.
- Lymphedema: Disruption of lymph nodes or prior node dissection increases arm swelling risks. Though mild cases are more common, chronic severe lymphedema can occur.
What’s the Risk of Infection as a Brachioplasty Complication?
According to Dr. Smith’s experience, the overall risk of infection after brachioplasty is relatively low, occurring in around 2% of patients. However, infection remains one of the most common major complications.
- Most surgical site infections happen within 30 days postoperatively. However, with prosthesis insertion, infections can occur up to 90 days later. Staph, Strep, and Pseudomonas bacteria are frequent causes.
- Risk factors that increase infection likelihood include obesity, diabetes, smoking, longer surgery times, and combining multiple procedures.
- Signs of a possible brachioplasty infection warrant urgent evaluation, including redness, swelling, increasing pain, warmth around the incision, fevers, and any wound drainage. Prompt antibiotic treatment provides the best outcomes.
While not common, infections must be caught early before advancing to become potentially serious.
How to Reduce Risk of Infection After Brachioplasty?

To reduce brachioplasty infection risks, Dr. Smith advises following all wound care instructions, monitoring for concerning symptoms like fever or incision redness, and promptly reporting any signs of infection for timely treatment.
Before Surgery
Take a thorough preoperative shower with antimicrobial soap to reduce bacteria on the skin.
Avoid shaving near the surgical sites to prevent micro-abrasions that can harbor bacteria.
After Surgery
- Strictly follow all post-operative instructions for incision care, activity restrictions, and compression garments. This supports proper healing.
- Keep the incision area clean and dry as directed.
- Practice good hand hygiene when caring for wounds.
- Attend all follow-up visits so Dr. Smith can monitor for proper healing.
Monitor for Signs of Infection
- Watch for increased redness, swelling, warmth, odor, drainage, or pain around the incision.
- Check for fevers over 101°F which may accompany an infection.
- Promptly report any concerning symptoms to the surgical team for evaluation and treatment.
What Are the Risks of Nerve Damage During a Brachioplasty Procedure?
The main nerves at risk of accidental injury during a brachioplasty are the medial brachial and medial antebrachial cutaneous nerves which can cause numbness, pain, and arm weakness according to Dr. Smith.
Nerve Injury Statistics
Published studies report an overall nerve injury rate of 2-5% in brachioplasty patients. While uncommon, nerve trauma remains one of the most concerning potential complications.
Causes of Nerve Damage
Nerves may be accidentally stretched, cauterized, cut or otherwise damaged during the dissection and flap elevation steps of a brachioplasty. Even minimal trauma to a nerve can lead to dysfunction.
Symptoms
- Numbness, tingling or burning sensations
- Sharp, shooting pain in the arm
- Weakness and reduced dexterity in the hands/fingers
- In severe cases, paralysis
Recovery Period
- Fortunately, most nerve damage is temporary as the affected nerves regenerate and heal over time.
- Complete recovery often takes weeks to months depending on the severity of the injury.
- Symptoms persisting longer than 3 months may indicate permanent neuropathy requiring further treatment.
Preventing Nerve Injury
- Meticulous surgical technique focused on visually identifying and avoiding key arm nerves helps prevent accidental damage.
- Careful wound closure avoiding excessive tension also minimizes risks of nerve trauma.
With Dr. Smith’s expertise, you can have youthful, beautiful arms you’re excited to show off. Let’s get started!
How to Manage Brachioplasty Problems at Home

To manage brachioplasty complications at home, Dr. Smith recommends elevating arms, icing, wearing compression garments, massaging swelling, watching for infections, protecting numb skin, taking medications as directed, and promptly reporting any concerns.
Preventing Infection
Closely monitor the incision sites for any concerning signs of infection like increasing redness, warmth, swelling, or purulent drainage. Fever can also indicate a developing infection.
Promptly contact our office if any worrisome symptoms arise. Strictly adhere to all prescribed oral antibiotics to prevent surgical site infections.
Controlling Swelling
- Keep arms continuously elevated above heart level when possible to minimize gravity’s effects.
- Apply cold compresses or ice packs for 15-20 minutes several times a day to reduce inflammation and fluid buildup.
- Wear your compression garment as directed by Dr. Smith to prevent swelling.
- Gently massage the arms to stimulate fluid drainage back into circulation.
- Stay well-hydrated and limit salt intake, which can worsen swelling.
Improving Bruising
- Cold therapy via ice packs helps minimize bruising discomfort and speeds resolution.
- Consider taking arnica supplements which may reduce bruising.
- Most bruising gradually fades within 2-3 weeks post-operatively.
Caring for Numb Skin
- Protect numb areas from injury and temperature extremes which could cause burns or wounds.
- Tingling and numbness typically resolve slowly over weeks to months as the nerves regenerate.
Closely following Dr. Smith’s at-home care instructions and attending all scheduled follow-up visits facilitate optimal recovery after brachioplasty.
Can Brachioplasty Complications Lead to Reoperation?
While most patients are satisfied with their brachioplasty results, Dr. Smith explains that complications occasionally require repeat surgery for correction.
Reoperation Rates
Published reoperation rates after brachioplasty vary widely in studies from 5% to over 20%.
The need for revision depends on the severity of the complications and response to nonsurgical treatments.
Reasons for Reoperation
- Residual skin laxity or contour irregularities (reported in about 40% of revisions)
- Hypertrophic scars unresponsive to conservative scar therapies (over 35% of cases)
- Recurrent skin loosening over time as patients age
Attempt Non-Surgical Treatments First
Many surgical complications like scarring or mild contour issues can improve with time and conservative therapies like:
- Silicone sheeting, compression, steroid injections
- Laser treatments and dermabrasion
- Massage and other scar treatments
Surgical Revisions
- If non-surgical options are ineffective, Dr. Smith may recommend revision surgery to address stubborn complications.
- Reoperations involve meticulous techniques to optimize the results.
- Realistic patient expectations are important when considering any revision procedures.
How to Minimize Scarring from Brachioplasty Complications
Silicone sheeting worn regularly for 4-6 months postoperatively reduces scar thickness, discoloration, and textural irregularities. Starting gentle scar massage at 2-3 weeks promotes mobility and softening. Applying sun protection prevents the darkening of healed incisions.
- Wearing compression garments for 4-6 weeks, using cold therapy early on, and keeping incisions clean facilitates ideal healing to minimize scarring.
- Laser treatments, micro-needling, and scar creams starting a few months after surgery further improve scar appearance.
From Dr. Smith’s perspective, strategic incision placement in natural contours and tension-reducing techniques aim to produce fine, discreet scars. We highly advise our patients to set realistic expectations as maturation takes 12+ months.
Can Liposuction with Brachioplasty Increase Issues?
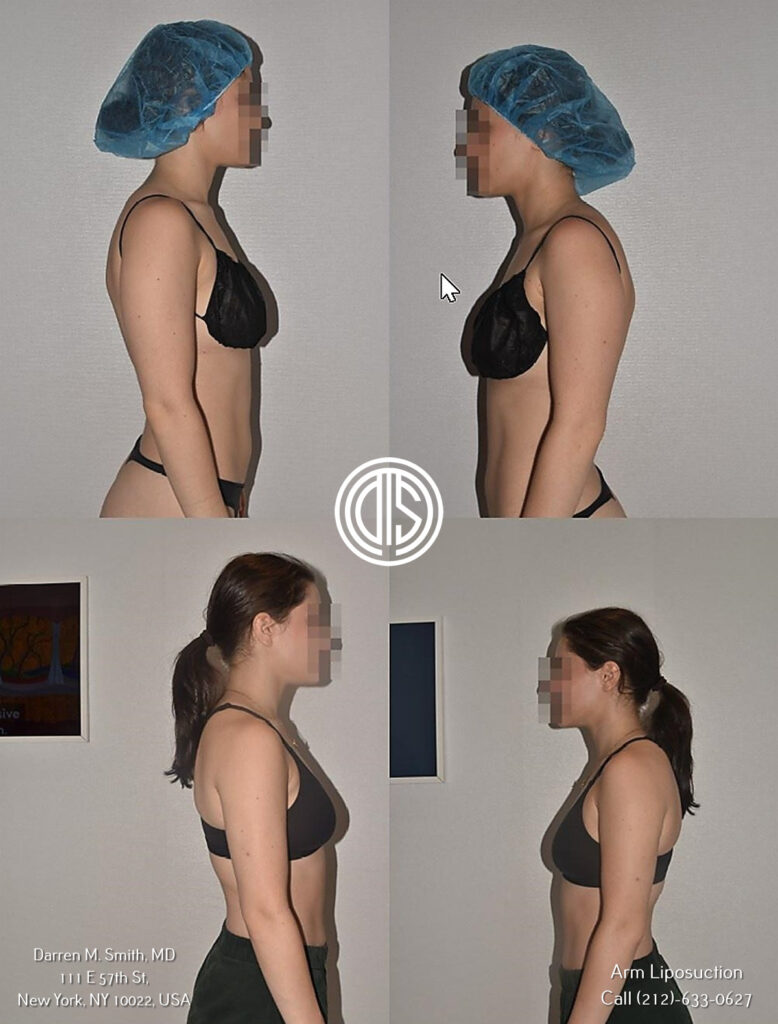
Several studies have found that liposuction can safely be combined with brachioplasty without increasing overall complication rates when performed correctly. One study found similar 9-10% revision rates with and without accompanying liposuction.
Potential risks of combining procedures include longer anesthesia exposure, fluid shifts, and challenges estimating optimal tissue removal. However, conservative, strategic liposuction adds minimal additional OR time in most cases. Avoiding over-resection is critical.
The combined approach allows simultaneous improvement of arm contour by addressing both loose skin and localized fat deposits. Patients tend to report higher satisfaction scores compared to brachioplasty alone.
In Dr. Smith’s experience, liposuction with brachioplasty is safe when done carefully by an experienced, Board-certified plastic surgeon. The dual procedure enables maximal arm rejuvenation in a single stage when appropriate.
See the amazing arm results Dr. Smith’s patients rave about – schedule your brachioplasty now!
FAQs
Can Exparel reduce pain and complications in brachioplasty?
Yes, Exparel provides effective pain relief after brachioplasty which can reduce the need for opioids and potentially lower complications, though individual results vary.”
What complications can occur after bilateral brachioplasty?
Common bilateral brachioplasty risks include poor scarring, bleeding, fluid buildup, nerve injury, wound issues, and arm mobility restrictions; risk rises with extensive procedures.”
Do brachioplasty complications affect arm movement?
Yes, brachioplasty complications like nerve damage, tissue injury, or poor healing can limit arm mobility; physical therapy often improves range of motion over time.
What anesthesia-related brachioplasty complications can occur?
Brachioplasty anesthesia risks include bleeding, breathing problems, nausea, blood clots, allergic reactions, but severe reactions are uncommon when protocols are followed.”
Are complications after brachioplasty higher in 2016 data?
Yes, a 2016 study found a 53% brachioplasty complication rate, much higher than more recent analyses showing rates around 30% or less.”
What is the rate of complications after brachioplasty in 2013 statistics?
A 2013 study showed a 31% brachioplasty complication rate, with hypertrophic scarring being the most common.
Can brachioplasty complications be found in Google Scholar research?
Yes, risks like nerve issues, wound problems, and scarring are well-documented in many published Google Scholar brachioplasty studies.
Complications were reported in 28.9% of over 1,000 brachioplasty patients reviewed in published studies on Google Scholar. The most common issues were hypertrophic scarring, fluid accumulation (seroma), and bleeding (hematoma).
Nerve damage is a known brachioplasty risk documented in Google Scholar research, occurring in up to 8% of patients. This can cause pain, numbness, and restricted mobility.
One 2016 study found an exceptionally high 53% brachioplasty complication rate, over double more recent analyses. This suggests surgical techniques and protocols have improved over time
Risk factors for complications identified in Google Scholar articles include extensive/combined procedures, high BMI, male gender, and medial incision placement.






